FraudLens
Automated pre-payment fraud/waste/abuse detection for healthcare payers
Private Fundraise
This company may be interested in raising funds from accredited investors. You must Request Access to see more information about this company.
Request Access 9 FraudLens Fast Facts
FraudLens Fast Facts
Fraudlens is a clinically intelligent fraud, waste and abuse (FWA) technology platform that provieds in excess of 3% FWA savings for healthcare insurance payers. It is designed for healthcare payers to find past, present and future FWA.
Key Highlights:
- Founded by Dr. Frank Din (dentist, informaticist and forensics expert), and Qasim Mueen (healthcare IT expert).
- Raised $1.085M in seed funding, $5.5M convertible debt.
- Developed dental solution and completed 8 proofs of concept.
- Working with our first dental solution client with "go-live" 5/15/21
- Developing medical solution and medical-dental crossover solution with 1 POC.
- Trademarked FraudLens, MedicaLens, and DentaLens.
- Completing patent application for clinically intelligent algorithm development.
- Mentioned in the Gartner Healthcare Report: Hype Cycle for US Healthcare as one of the payment integrity solutions to watch for in the coming years.

 The Big Problem
The Big Problem

The $3.8T U.S. healthcare industry comprises as much as $760 B in fraud, waste and abuse (FWA) that isn’t being detected today. The current solutions to detect FWA are not solving the problem.
Two problems continue to plague the integrity of the insurance company's payment process;
1. Payers' move to an auto-adjudication process that pays claims fast - - without reviewing,
2. Payers conducting only manual reviews of approximately 10% of the largest claims - - after they have already paid the provider.
Both problems leave 90% of claims untouched or paid inappropriately.
FraudLens is the only company focusing on the Right Payment Methodology
 Solution: The Right Payment Technology
Solution: The Right Payment Technology
 Identify Confirm Prevent Eliminate
Identify Confirm Prevent Eliminate
FraudLens technology contains over 1M configurable rules and clinically intelligent algorithms that analyze all claims to uncover new issues not possible with traditional FWA processes.
FraudLens analyzes all payer claims including low-dollar, high-volume and highly-repetitive claims that competitors don't review resulting in recommendations of which claims to pay, which to reject and which to review.
By reducing inappropriate payer costs, FraudLens saves 3-5% of the insurance payer’s total claim amount spent.
This is The Right Technology!
 How FraudLens Works
How FraudLens Works
The payer sends FraudLens claims data that have been fully adjudicated and ready for payment. The FraudLens platform runs the data through our clinically intelligent algorithms and business rules exposing FWA.

 FWA Insurance Payer Market
FWA Insurance Payer Market
- FraudLens' target healthcare client for our SaaS business model is a medium-sized insurance company .
- FraudLens will be targeting the top 50 health and top 50 dental plans for our licensing business model.
- There are 290M dental insurance consumers and 300M medical insurance consumers covered by various insurance programs in the U.S.
- FraudLens' detectable FWA in the healthcare market is $14B or 3% of the total estimated FWA.
- FraudLens shares that savings with the insurance payer. FraudLens' 20% shared savings is $2.8B.
- FraudLens' addressable FWA market is estimated at 3% of that shared savings or $72M per year.
 Healthcare Payer Benefits
Healthcare Payer Benefits
- Outperforms rules-based systems and improves FWA and error detection;
- Uses in-depth analysis to understand and present FWA patterns, trends and anomalies in an easy-to-understand format;
- Our post adjudication - prepay model does not disrupt current claim payment processes;
- Configurable, applying clinical code edits with specific and unique business rules to reflect each line of business for each client;
- Eliminates false positives which ultimately results in manual intervention;
- Fraudlens is able to process all claims, including low-dollar / high-volume claims rather than the traditional low-volume / high-dollar claims;
- Maximizes SIU productivity by automatically presenting the largest and most complex issues to investigators for pursuit;
- Could be used post-pay or at any position in the payment process;
- Increases claim through-put resulting in lower administrative cost of claims processing; and
- Provides the payer with a higher ROI than any other competitor.
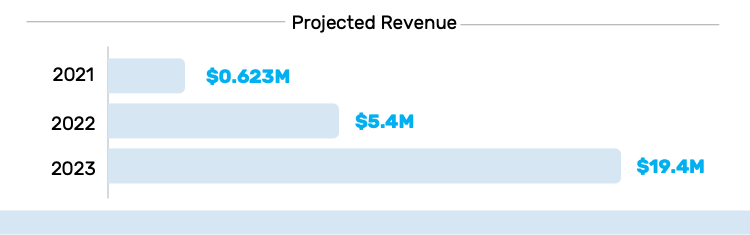
 Business Model
Business Model

Shared savings: 20 - 25% of the savings actually received by the client. FraudLens only gets paid when our technology performs.
License fee: Tfor the exclusive use of our technology installed behind the payer's firewall allowing them to get the right technology inside.
 Meet The Team
Meet The Team
 Qasim Mueen, Chief Executive Officer and Co-Founder
Qasim Mueen, Chief Executive Officer and Co-Founder
Founder of Zigron IT Services company focusing on IoT applications. Zigron Healthcare (acquired by Stella Tech. 2016), co-founder of TransparentHands.com
 Kashif Mueen, Chief Technical Officer
Kashif Mueen, Chief Technical Officer
Former CTO of Zigron Healthcare (exited 2016), CTO Wherever TV (IPO), 20+ years experience as an enterprise architect, product and platform development, R&D.
 Michel Heitstuman, Chief Operating Officer
Michel Heitstuman, Chief Operating Officer
Entrepreneur with 20+ years experience in start-ups and multinationals; 9 yrs in sales with IBM, co-founder AOL Enterprise, CEO Brazil & VP Global Strategy Upaid Systems.
 Robert Steele, Chief Sales and Marketing Officer
Robert Steele, Chief Sales and Marketing Officer
20+ years in the healthcare payment integrity business, understands the value of teamwork, building relationships and driving value both internally and with customers. Closed over $750 million in Total Contract Value, called relentless by his colleagues.
 Yoemy Waller, Vice President of Integration
Yoemy Waller, Vice President of Integration
Long-term healthcare IT professional and data scientist with 20+ years experience in project management, big data, clinical and dental informatics, population health, and bioinformatics.
 Javed Iqbal, Vice President of Technology
Javed Iqbal, Vice President of Technology
Working directly with the founders, Javed was the solution architect that led the team developing the intelligent analytic fraud solution for FraudLens. 12+ years guiding teams through all phases of software development; system architecture & design, IT software.
The Business Plan area is locked. You must Request Access to this company to see more information including the Business Plan.
Request Access
N
No updates yet.
%
No backers yet.
Quick Signup TBD
You must have an account to do this!
